
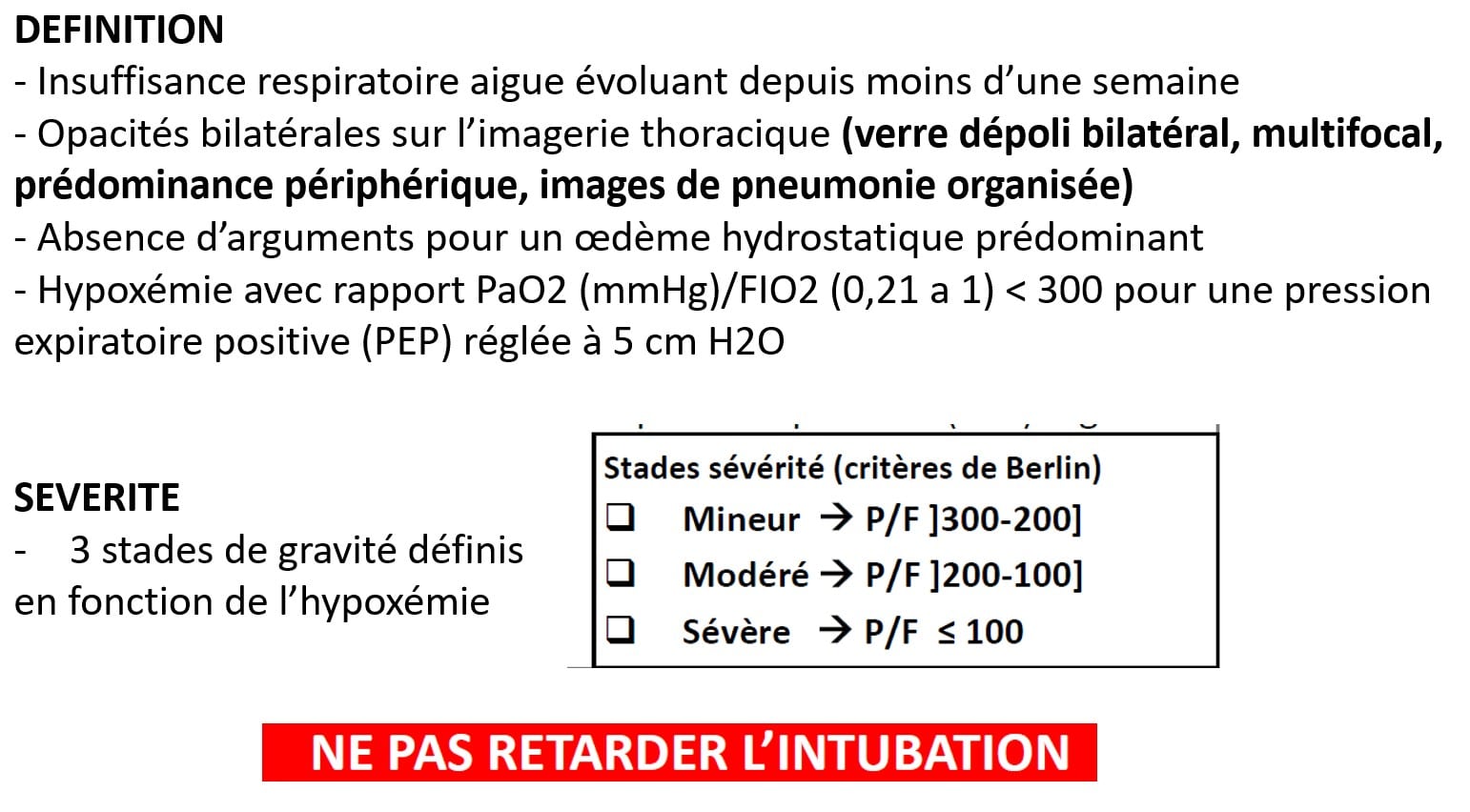
This ensures the “balloons” that are the alveoli do not fully empty, and that residual volume we talked about in Chapter 1 is left in the lungs to make them easier to blow up for the next breath. PEEP is, at minimum, always set to 5cmH20. We set the ventilator to have PEEP to replace the air that is normally left in the lungs. Utilizing positive pressure from a ventilator eliminates this ability and must be artificially added via the ventilator. Remembering the pressures noted in spontaneous breathing, the negative pressure in the pleural space ensures some air is maintained in the lungs to keep them inflated. When we move to mechanical ventilation and switch to positive pressure in the lungs, we need to ensure the lungs do not fully empty at the end of exhalation. As you may have already surmised, the PEEP setting on the ventilator is meant to mimic the physiologic properties that occur when spontaneously breathing. As we begin to discuss mechanical ventilation, PEEP is also set on the ventilator. In Chapter 1, we learned that Positive End Expiratory Pressure (PEEP) describes the little bit of air that remains in the alveoli after exhalation has ended. There is another factor that can affect oxygenation, and this factor becomes extremely important when it applies to ventilation and specifically ventilating potentially sick individuals with lung pathologies. In those with PEEP i, increasing ventilator PEEP to offset PEEP i improves synchrony.īronchopulmonary dysplasia critical care mechanical ventilation.At this point in your learning, you should understand how increasing the FiO 2 can directly impact the amount of oxygen available to the body through the oxygen content equation-specifically hemoglobin amounts and SpO 2. PEEP i is measurable in infants with sBPD with concurrent esophageal manometry and flow-time tracings without the need for pharmacological paralysis. No adverse events occurred during testing. Conditional sedation was reduced in five infants postprocedure. For the eight infants requiring an increase in set PEEP, there was an 18.9% reduction in WE and a reduction in FiO 2 (0.084 ± 0.058) requirements in the subsequent 24 hours. Eight infants required an increase, one, a reduction, and three, no change in the set PEEP. Mean baseline ventilator PEEP was 16.4 cm H 2 O (14-20 cm H 2 O). Twelve infants were assessed (gestational age, 24.9 ± 1.4 weeks study age, 48.8 ± 1.5 weeks, postmenstrual age). Sedation requirements evaluated 72 hours preprocedure and postprocedure. FiO 2 and SpO 2 measured pre- and post-PEEP adjustment. "Best PEEP" was the setting with minimal wasted efforts (WE), an inspiratory effort seen on the Pes waveform without a corresponding ventilator breath. The set PEEP was adjusted to minimize PEEP i. PEEP i defined as the difference between Pes at start of the inspiratory effort minus Pes at onset of inspiratory flow. PEEP i measured by esophageal pressure (Pes) and pneumotachometer, during pressure-supported breaths.
Interventional study in infants with sBPD. To determine if PEEP i is present in infants with sBPD during spontaneous breathing and if adjusting ventilator PEEP improves patient/ventilator synchrony and comfort. Infants with severe bronchopulmonary dysplasia (sBPD) and airway obstruction may develop dynamic hyperinflation and intrinsic positive end-expiratory pressure (PEEP i ), which impairs patient/ventilator synchrony.


 0 kommentar(er)
0 kommentar(er)
